
A broad range of visual field and radiographic findings are identified, a consensus on treatment of neuromyelitis optica spectrum disorders and anti-MOG positive optic neuropathies has yet to be accepted but initial high dose immunosuppression followed by low dose maintenance therapy is favoured.Īnti-aquaporin 4 anti-myelin oligodendrocyte glycoprotein antibody neuromyelitis.
-Immunohistochemistry-Paraffin-NBP2-66957-img0002.jpg)
No correlation between initial VA or RNFL and final visual outcome is identified. Visual field testing and radiological findings for each group are described. No correlation was seen for initial RNFL thickness and final visual outcome in this group either. The same statistical analysis was performed for the correlation between retinal nerve fibre layer (RNFL) and VA and similar outcomes were observed. There was no statistically significant correlation (Pearson correlation) between GCL thickness and presenting and final VA. Nine of the 16 patients were female and the average age of onset was 29.2y in the MOG group and 42y in the AQP4 group. Initial and long-term treatment is also summarised.Ī total of 16 patients were included in the study consisting of 12 anti-MOG and 4 anti-AQP4 positive patients.
Optical coherence tomography (OCT) scanning was preformed to examine the correlation between ganglion cell layer (GCL) thickness and visual acuity (VA) at presentation and as a determinant of final visual outcome in both groups. Structured clinical exam and multimodal imaging was undertaken sequentially on each. Clinical findings including presence of a relative afferent pupillary defect, colour vision and disc assessment were recorded. Each of these patients had clinical signs and symptoms of optic neuritis and consisted of all patients who had a positive blood antibody result in our centre.
ANTI MOG ANTIBODY SERIES
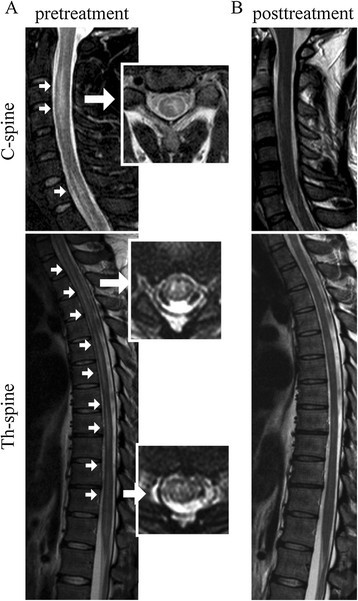
MOG antibody associated demyelination may mimic the findings described in COVID-19 encephalopathy.To describe the clinical characteristics and treatments associated with antibody positive optic neuropathies including anti-myelin oligodendrocyte glycoprotein (MOG) and anti-aquaporin 4 (AQP4), alongside diagnostic modalities, investigations, and outcomes.Ī cross-sectional single-centre retrospective case series consisting of 16 patients including 12 anti-MOG positive patients and 4 anti-AQP4 positive patients. Conclusion: In the advent of the COVID-19 pandemic, it is important not to attribute clinical findings to SARSCov-2 without excluding other disorders. It is likely that SARSCoV-2 triggered off an inflammatory process in this child mediated by MOG antibodies. Our child did not have any feature to suggest PIMS-TS. Lesions in the splenium of the corpus callosum appear to be a relatively consistent finding in children with PIMS-TS. Discussion: In literature, there is a paucity of information regarding COVID-19 related encephalopathy. Her anti-MOG antibodies were later found to be positive, which explains the symmetrical scan changes and brainstem involvement. She made good progress with steroid therapy and at discharge, was able walk a few steps, recognise voices, clap at nursery rhymes, eat and drink normally, but had cortical visual impairment, which is improving.

This was initially felt to be in keeping with Covid-19 encephalopathy, especially given the presence of the splenial lesion. Diffusion restriction with T2/FLAIR signal change was noted in the thalami and pons. MRI brain showed bilateral widespread T2 and FLAIR signal changes of subcortical white matter and the splenium. CSF investigations were normal, including a negative SARSCoV-2 RNA. PCR nasal swabs revealed the child was SARSCoV-2 and Adenovirus positive. She required intubation, was started on intravenous antibiotics, Aciclovir and Levetiracetam and was transferred to PICU. Case A previously healthy 1 year old girl presented with reduced GCS, decorticate posturing, seizures and a 3-day history of fever. We describe a case triggered by SARSCoV-2. ABSTRACT Introduction: Acute disseminated encephalomyelitis (ADEM) is a rare autoimmune disease involving inflammation of the brain and spinal cord, usually triggered by a preceding illness or vaccination.


 0 kommentar(er)
0 kommentar(er)
